There is a postpartum care crisis in America.
April 11-17 is Black Maternal Health Week.
April 11-17 is recognized as Black Maternal Health Week, which aims to raise awareness of maternal health inequities and empower Black mothers and families by focusing on advocacy for improved outcomes.
An interview with Dr. Venice Haynes, from the United States of Care
Recently, I had the pleasure of interviewing Dr. Venice Haynes from United States of Care. Haynes is a social and behavioral scientist with over 15 years of public health experience.
Q: What exactly is The United States of Care?
A: It is a not-for-profit organization that attempts to ensure that everyone has access to quality, affordable health care regardless of health status, social need, or income. USofCare hopes to expand access to quality, affordable health care in the near term while paving a path toward durable, people-centered federal policies that achieve that mission. USofCare envisions a health care system that provides people with high-quality, personalized care that meets their unique needs at an affordable price.
Q: Dr. Haynes, can you tell me about your career and your training?
A: My research has focused on addressing social determinants of health, health disparities, and health equity in underserved populations. I have both a master’s degree and a PhD in Public Health. Currently, I serve as the Senior Director of Health and Community Engagement for USofCare, where I am leading the organization’s listening and research work to understand the changes mothers and families want and need from the health care system.
Q: Why is USofCare interested in the postpartum care crisis in the United States?
A: There is a postpartum care crisis in America. Despite being a high-income nation, America’s maternal mortality rates are extremely high, and this fact highlights significant gaps in postpartum support in the U.S.
Background information about maternal and infant deaths
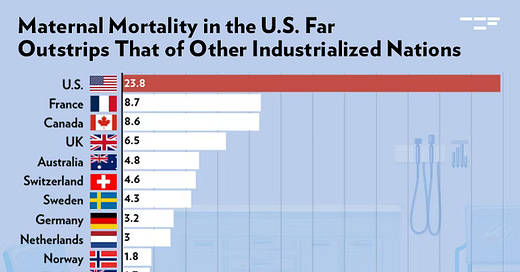
The current maternal mortality rate is ten times higher in the U.S. than other high-income countries. In 2022, the U.S. experienced 22 maternal deaths for every 100,000 live births. Norway, Switzerland, Australia, the United Kingdon, and Canada all had less than 9 maternal deaths per 100,000 live births!
Fifty-five percent of maternal mortality occurs in the postpartum period. The mortality rate is highest for Black women. Some speculate that 80% of maternal deaths in the U.S. are preventable. The gap between the U.S. and other countries’ maternal death rates are most likely due to 1) differences in health insurance, 2) the use of midwives, and 3) available paid parental leave.
In the U.S., Medicaid is the single largest payer of maternal care services, covering 41% of all births in 2022, according to the CDC. Federal law requires Medicaid to provide up to 60 days of postpartum coverage, though some states have extended that coverage period to 12 months.
For the forty to fifty percent of mothers that have private, employer-based insurance coverage, their coverage varies a great deal. Is the lactation consultant covered, is the breast pump, and how about the Doula? What about psychotherapy and antidepressant medication for PPD should it occur? Will those be covered?
In 2023, only 27% of private industry workers had access to paid family leave, according to the U.S. Bureau of Labor Statistics. In addition, in the U.S., we do not use midwives in a way other countries are using them. Other countries have really integrated midwives into their health care system, but in the U.S., it’s a different story.
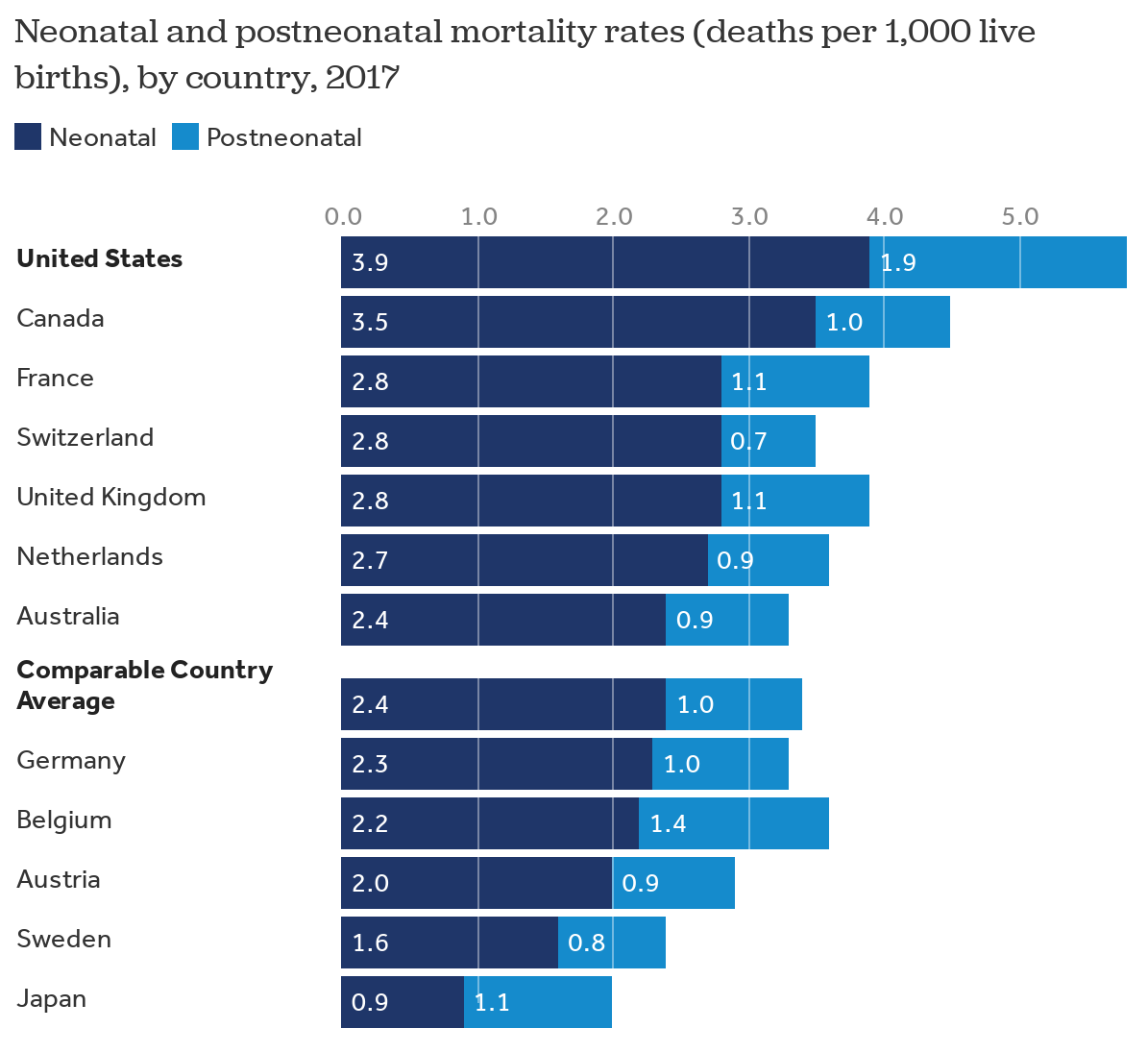
The U.S. infant mortality rate (5.6 deaths per 1,000 live births in 2022) is higher than many other high-income countries, ranking 33rd out of 38 OECD countries. (OECD = intergovernmental organization for economic cooperation and development.)
And, since the Dobbs decision, there has been an increase in infant mortality rates. Take the situation in Texas as an example: between 2021 and 2022, infant deaths in Texas rose from 1,985 to 2,240. This is a 12.9 % increase in infant deaths in Texas versus a 1.8 % increase in infant deaths in the rest of the U.S. during the same period. (Infant deaths were those under 12 months old.) It is believed that the strict Texas abortion ban (SB 8) impacted infant deaths in the state. Congenital anomalies, which are the leading cause of infant death, increased in Texas, but not in the rest of the U.S.
Back to my interview with Dr. Haynes
Q: What is “The 100 Weeks Project”?
A: It is an initiative designed to transform postpartum care by providing comprehensive, personalized support from conception through the first year postpartum. This initiative addresses the physical, mental, and social needs of mothers, fathers, and families.
The concept of “forty weeks” misses many of the issues that new moms face. It doesn’t capture the time before getting pregnant, her experiences during pregnancy, labor and delivery, nor the time after giving birth. Currently an average U.S. mother is discharged from the hospital, and she is not seen again for three weeks, and after that she may be without a support system during her recovery and period of matrescence (or becoming a mother).
Q: How is “100 weeks” a better concept to envision?
A: The concept of “100 weeks” considers a mother’s entire pregnancy journey, from pre-conception (4 weeks) through pregnancy (40 weeks) through the first year (52 weeks) and one more month; this is 4+ 40 + 52 + 4 = 100.
Q: Which practices do the “100 weeks project” hope to elucidate?
A: Our current health care system is not set up to support postpartum care, and health care coverage is fragmented. USofCare aims to create solutions that ensure every pregnant woman has access to and coverage of postpartum care services regardless of her health care coverage.
Q: How does the “100 weeks project” work exactly?
A: We have interviewed sixty women – from rural, suburban, and urban locations, from all socioeconomic levels - about their pregnancy journey. We learned about their challenges along the way - their highs and lows, their stressors, and the barriers that women experience - and what bright sports they encountered. We heard about the emotional toll of navigating the healthcare system, particularly for those facing early motherhood struggles.
Q: Can you tell us about the journey map that USofCare is creating?
A: We have identified obstacles and challenges for moms during each phase of these 100 weeks. The picture these women have painted for us is not pretty:
In the preconception period, these include struggles with infertility, unintended pregnancy, and access to birth control.
During the pregnancy period there are other obstacles, such as prenatal care inadequacy, vitamin deficiencies, ectopic pregnancy diagnosis, abortion counseling, miscarriage, gestational diabetes, and preterm labor.
During the childbirth and labor period we heard about poor quality birth location, traumatic birth experiences, stillbirths and miscarriages, unequal pain treatment, increased tendency for C-section, and racial profiling and prejudice in L&D.
Describing their problems during the postpartum period, these mothers told us about breastfeeding stigma, low quality NICU care, postpartum care inaccessibility, lack of lactation consultation services, lack of maternity or family leave, lack of postpartum insurance coverage, lack of care for PPD, unintended pregnancies, and return to work uncertainty. Moms were consistently searching for support!
Q: Were there any bright spots discovered along their journey?
A: Yes, some moms felt they had good OB care, very supportive pediatricians, lactation support services, and employers who provided some maternity leave. Some black moms were aware of and felt supported with the New York Times publication “Protecting your Birth: a Guide for Black Mothers” published in 2020.
Many moms were aware of and used the Irth app which allowed them to review their doctor and hospital care. Mothers felt that this app empowered them to share satisfaction and care experiences and give feedback to other moms and local hospitals.
Q: What are the next steps for the “100 Weeks Project”?
A: Women told us they need more support after their pregnancy and during the postpartum period, where they felt their care from health care providers was severely diminished. Improving care during the postpartum period, when most maternal deaths occur, can reduce maternal mortality and morbidity and lay the foundation for better physical, mental, emotional, and social well-being for the mother. This can improve the overall maternal health experience.
USofCare has developed a “Vision for Postpartum Care“ that describes a health care system in which postpartum women receive personalized, comprehensive care that empowers them to have a joyful postpartum experience. Please see their website for additional detailed information.






We are going so far backwards under the current reign of terror imposed by primarily WPMs.